Addressing the gap – equality and equity in healthcare
The NHS was set up 75 years ago to improve the health of the UK population and to reduce inequalities in healthcare – to make healthcare available and accessible, free of cost, to all. There wasn’t anything like it at the time. In the next of our series of articles celebrating the 75th anniversary of the NHS, Partner, Head of Office in Wales and the Public Law Group, Eve Piffaretti discusses the challenges presented by health inequality and how they are being tackled.
Fast forward three quarters of a century, and despite the existence of the NHS health inequity persists with the UK seeing growing health inequalities. There have been a series of major reports focusing on inequity and inequality in health access and outcomes in the UK, such as the Black Report, published in 1979, the 2010 report of the Marmot Review Fair Society, Healthy Lives, further reviewed, just before the COVID-19 pandemic. Equity in England: The Marmot Review 10 years On, presented a picture that was not encouraging, suggesting that policies of austerity had seen health disparities increase, with the gap between those with the best and worst health and wellbeing widening. The COVID-19 pandemic as well as the cost of living crisis has amplified these inequalities further. Those who continue to face disadvantage, include peopling living in areas of high socio-economic deprivation, those with protected characteristics, such as disability, age and ethnicity and those from inclusion health and vulnerable groups, as well as geographical factors face health disparities.
Health inequity and health inequality
These are two distinct concepts:
- Equality – means ensuring that everyone gets access to the same resources.
- Equity – means ensuring that everyone has the opportunity to get the same outcome, with resources distributed according to need.
The two are closely linked when it comes to healthcare. The World Health Organisation (WHO) defines health inequalities as “differences in health status or in the distribution of health determinants between different population groups”. Reducing health inequalities improves life expectancy and reduces disability across the social gradient. Consequently, tackling health inequalities is core to improving access to services, health outcomes, improving the quality of services and the experiences of people. It is also core to the values and purpose of the NHS.
The domains of health inequality have been highlighted in a UK Government report, ‘Health disparities and health inequalities: applying All Our Health’, from which the image below has been sourced.
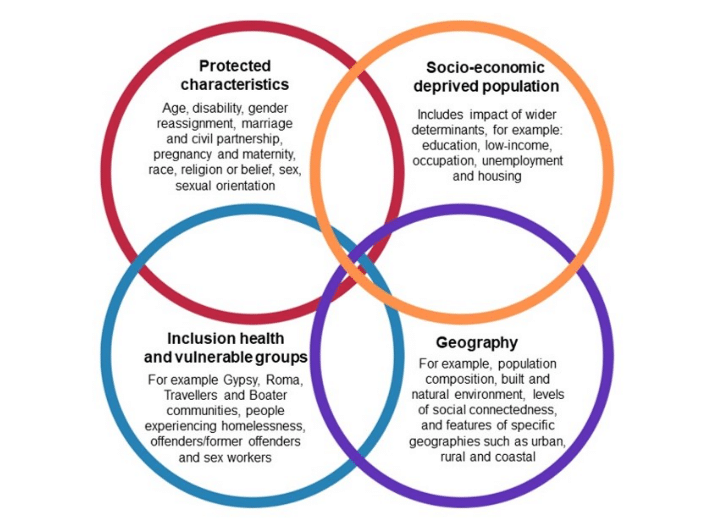
The domains of health inequality (adapted from Health inequalities: place-based approaches to health inequalities).
Although a great deal of work is underway within health and care organisations it is more crucial than ever to prioritise equity of access to services for all citizens, to tackle and reduce inequality and ensure fair outcomes. The focus on addressing the wider social determinants of health – has been on government and civil society. However, health inequalities are the result of many and varied factors and the NHS alone does not hold all the levers required to create the necessary conditions for good health and wellbeing. Everyone has a role to play in this, including businesses who “can make a difference by introducing good employment practices, through their goods and investments, and through the impact they have on communities and the environment.” We have a role to play in personal responsibility for our own health and wellbeing.
The UK Government has confirmed that the planned Health Disparities White Paper will not be going ahead, instead, it will publish a Major Conditions Strategy, with an interim report due to be published this summer, following a call for evidence. Health disparities and health inequalities: applying All Our Health guidance has been published aimed to help health and care professionals and the wider workforce in England prevent ill health and promote wellbeing as part of their everyday practice.
In Wales, The Welsh NHS Confederation’s Health and Wellbeing Alliance has called on the Welsh Government to produce a cross-government plan for reducing poverty and inequalities in adults and children, outlining the action being taken across all government departments, accompanied by guidance on how individual organisations should collaborate to reduce inequalities and tackle the cost-of-living crisis.
What's stopping change?
Tackling the causes and consequences of health inequalities is a central priority for health and care systems in the UK and a legal drivers in the form of citizen’s rights and statutory duties apply. The key founding principles of the NHS have been built upon by legal duties including the Human Rights Act 1998 and the Equality Act 2010. The latter through its Public Sector Equality Duty, requires public sector bodies, including the NHS to have due regard to the needs to eliminate discrimination, harassment and victimisation, to advance equality of opportunity, and to foster good relations between people who share a relevant protected characteristic (as cited under the Equality Act 2010) and those who do not share it.
In addition, in England the National Health Service Act 2006, as amended, requires due regard to be given to the need to reduce inequalities between patients in access to, and outcomes from healthcare services and to ensure services are provided in an integrated way where this might reduce health inequalities. In 2022, further provisions were introduced by the Health and Care Act 2022 included a statutory performance and reporting framework including health inequalities and promotion of integration and partnership-working to improve health and tackle health inequalities. Working in partnership with people and communities: Statutory guidance reinforces the importance and positive impact of working with people and communities and that NHS England, Integrated Care Boards and NHS Trusts have legal duties to make arrangements to involve the public in their decision-making about NHS services, as well as the new ‘triple aim’ of better health and wellbeing, improved quality of services and the sustainable use of resources.
While involving people and communities is a legal requirement, working with them also supports the wider objectives including population health management, personalisation of care and support, addressing health inequalities and improving quality. The legal duties provide a platform to build collaborative partnerships that start with people and focus on what matters to communities.
Building on this and contributing to the UK government’s levelling up agenda, NHS England has issued the Core20PLUS5 approach to support focused action on improving health inequalities, both at a national and system level. This approach is focused on action in the following areas. Furthermore the NHS England Healthcare Inequalities Improvement Programme aims to drive this forward with the vision of delivering exceptional quality healthcare for all, ensuring equitable access, excellent experience and optimal outcomes. For more information see the Equality and Health Inequalities Network NHS future forum space.
In Wales over the past decade, the Welsh Government has passed the Wellbeing of Future Generations (Wales) Act 2015 (‘the Act’) the Public Health (Wales) Act 2017 (including health impact assessments which have not yet been introduced) and has enabled the Equality Act 2010’s socio-economic duty. The Act gives specified public bodies across Wales the statutory duty to improve the social, economic, environmental and cultural wellbeing of Wales – the Wellbeing Duty. The Act also tells these organisations that they must go about meeting this duty by following the sustainable development principle that “seeks to ensure that the needs of the present are met without compromising the ability of future generations to meet their own needs.” Under the Act, public bodies will also need to show that they have applied the sustainable development principles, or Five Ways of Working in going about their work. It sets out seven long-term well-being goals, including a healthy Wales, a resilient Wales, a prosperous Wales, a more equal Wales, a Wales with vibrant culture and cohesive communities, and a globally responsible Wales. The Act also established an independent commissioner to oversee implementation.
Collaboration and communication are key
It’s clear that a long-term approach is required to tackle entrenched inequalities between and within places across the UK. The NHS cannot do this alone. Wider determinates of health – poverty, discrimination, educational attainment, employment and housing – relate to barriers that the NHS by itself cannot overcome. Collaboration brings an opportunity to capture a holistic view of inequalities and work with people and communities. Local authorities and other partners are well placed to understand the social determinants of health and how they can be addressed together and the legal frameworks in place in England and Wales both promote and require this.
While the approaches to working with people and communities depend on the specific context, there are some key considerations that apply which meet the legal duties and ensure that people are supported to take part.
Whichever approach is taken, it needs to be fair and proportionate. Judgment is needed and it is not an area where definitive advice can be offered without knowledge of the specific circumstances. Where staff need to make a particularly complex or potentially contentious decisions, they need to ensure that they comply with the legal duties which apply, some of which have been flagged above.
There are some important actions to take to ensure this is delivered:
- 1. Consulting the patients
Making sure that people are involved by consulting, providing information or in other ways. Getting them involved is crucial. The patient has to have a voice. Providing a service around what is actually needed, rather than what organisations think might be needed.
- 2. Tapping in to expertise and knowledge
Collaboration and communication with organisations that represent protected, inclusion and vulnerable groups, is also important to ensure that the services provided can respond to the needs of the people that they are providing them to.
- 3. Communicating how to get support
There is a need for the health service to take people with them on the journey, as they implement changes to systems and services. Patients are the key to everything so ensuring timely communication of any change will help ensure that they take hearts and minds with them. The move to increased digital inclusion has benefits for society as a whole as well as for the NHS. It can support local health and care priorities and how policy is supporting the agenda and is important to take these benefits into consideration when considering the impacts for public health.
How can Blake Morgan help?
It can be complex for organisations to know exactly what action they need to take to meet their legal duties, so often there is a need for external advice. Blake Morgan has the experience to advise on these legal duties and help organisations to do everything they can to tackle inequalities.
Enjoy That? You Might Like These:
articles
articles
case-studies